September 30, 2021
The Live Oak Project is a coalition of experienced advocates and innovators working in collaboration with Pioneer Network, a national leader in the culture change movement. We are on a mission to re-imagine, redesign, and transform long-term services and supports in America so that each person can thrive.
We share a vision for a transformed culture of long-term services and supports rooted in basic human rights, one that cultivates well-being, relationships, and community through empowerment of each person and each group of stakeholders.
We are leading a multigenerational grassroots movement made up of everyday Americans who share our passion – elders, people living with disabilities, people living with dementia, including Alzheimer’s, family care partners, and professionals including the direct care workforce – all joining together to ask government leaders to think bigger and bolder to fund and champion innovative solutions within our communities.
“Building and sustaining momentum for change requires large amounts of positive affect and social bonding – things like hope, excitement, inspiration, caring, camaraderie, sense of urgent purpose, and sheer joy in creating something meaningful together.”
– D.L. Cooperrider & D. Whitney,
Appreciative Inquiry: A Positive Revolution in Change
As a coalition, we join other advocacy groups in supporting many elements of legislation now before Congress that address increased wages and benefits for direct care workers and funding to support small house/household models to replace the traditional, institutional nursing home.
However, as innovators with decades of experience, we believe nursing homes need more than improvement. They require urgent and profound transformation – from institutions to real homes that support the well-being of all who live and work within.
We believe commitment to such transformation must happen now, as part of the larger investment in long-term services and supports being considered by congressional committees through the budget reconciliation process.
Ageism and ableism are root causes of our underinvestment in system transformation. Ageism alone is estimated to cost the U.S. health care system $63 billion annually.1 The Live Oak Project coalition is dedicated to combatting ageism and ableism in all forms as a matter of social justice. As such, we advocate for significant investment in three areas:
1. STAFFING
COVID-19 has exacerbated the imperative for significant investment in direct care workforce wages, benefits, and training. These essential caregivers have continued to do their job during the pandemic, despite clearly documented and avoidable risks to the health and mortality for themselves and their families. Sadly, nursing homes have lost 380,000 workers since February 2020.2 Staff shortages, further exacerbated by COVID, have created a crisis in health and long- term care. Swift action is needed to support the direct care workforce across all long-term services and supports settings so that those in need will receive care.
We advocate for:
-
$55 billion to increase Medicaid reimbursement for nursing homes as a direct pass-through to pay wages and provide benefits that enable them to recruit and retain full-time staff, especially certified nursing assistants and nurses who promote socialization, agency and empowerment of elders and people living with disabilities, including people living with dementia. Full accountability and transparency from nursing home chain ownership as well as individual nursing homes must accompany new funding.
-
$1 billion investment in aging services workforce systems to implement strategies that strengthen recruitment, career, and training opportunities for our nation’s direct care workers. Taking care of the direct care workforce will result in improved quality of care and quality of life for the residents as well as the staff.
2. ARCHITECTURE
COVID demonstrated small is better when it comes to nursing home living environments, and the importance of private rooms and baths, good air circulation, and ample communal space cannot be overstated.
Medicare and Medicaid will spend $1 trillion on institutional nursing home care between 2022 and 2028.3 The proposed $1.3 billion small house/household demonstration program is well intentioned. However, with individual nursing homes eligible for up to $39 million in transformation funds, the demonstration could lead to as few as 33 additional small house/ household developments — adding just 10% to the existing capacity of such developments around the country. Substantially greater funding would provide the data and incentive to drive the total reimagination, redesign, and transformation of nursing homes particularly for those receiving Medicare and Medicaid.
We advocate for:
-
A dedicated Federal Medical Assistance Percentage (FMAP) increase for states to spur new congregate care model development as part of Medicare-Medicaid integration efforts and in alignment with the proposed FMAP increases for home and community-based services.
-
Broadening the five to 14-person limit per small house. There are small house/households of 10-20 persons operating successfully. We recommend further study before codifying size parameters of models.
-
Further study to explore options that eliminate barriers to innovation, such as low interest loans for capital for nursing homes to upgrade their physical plants.
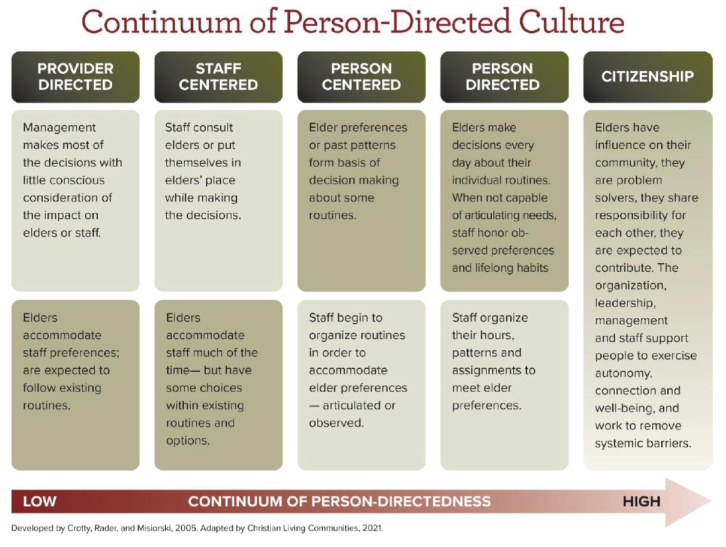
3. CULTURE Our nation’s experience implementing the Nursing Home Reform Act of 1987 has demonstrated the limits of attempting to de-institutionalize services and individualize care through regulatory oversight alone. Transforming institutions into person-directed, relationship-centered, livable communities requires sustained investment in new infrastructure and approaches. We must build age-friendly ecosystems focused on what matters to elders and those closest to them, no matter the setting – where all have access to a meaningful life and activities that strengthen each person physically, socially, and intellectually.

Lack of sufficient funding at all levels, as well as how funding is allocated and how those receiving funds are held accountable, is at the core of the challenge, but on a deeper level, the whole system must be reimagined, redesigned, and transformed – from the hallways of CMS to each state survey agency, to what happens in each person’s residence and in each community. The United States has spent billions on a regulatory process that is often counter- productive to innovation and has spent virtually nothing on supporting person-centered care and the culture that promotes practices that are mandated by existing laws and regulations, including:
1987 Nursing Home Reform Law which was included in the Omnibus Budget Reconciliation Act (OBRA ’87). It established quality standards for nursing homes nationwide and preserved residents’ rights. It emphasized the importance of quality of life, not just quality of care.
1995 Federal enforcement regulations for OBRA ’87 passed.
2010 A key directive of the Affordable Care Act was to transform both institutional and community-based long-term care into a more person-centered system.
2016 CMS issues a comprehensive revision of the federal nursing home regulations to reflect substantial advances that have been made in theory and practice of service delivery and safety. Person-centered care and quality of life are important themes integrated throughout the new regulations and interpretive guidance.
Despite the resistance of the system, as innovators and advocates we have developed expertise in incubating life-affirming, humane demonstrations that are cost-effective and efficient. Our efforts have been grounded in a common culture that promotes the dignity of each person, community development, continuous learning, and the empowerment of the human spirit.
The promotion of this culture is vital not only in nursing homes and other congregate settings, but also across the spectrum of home and community-based services – wherever someone calls home. Growth of home and community-based services alongside unprecedented population aging in neighborhoods creates new challenges and opportunities.
We advocate for:
-
Robust and immediate investment in education for federal and state regulators to empower the creation of person-directed, relationship-centered, livable communities with active citizenship among residents who have influence as problem solvers, sharing responsibility for each other with expectations to contribute. Regulators must support communities where people are supported to exercise autonomy, build connection, and foster well-being – and where all work together to remove systemic barriers. We also recommend further study and investment in making the regulatory process consistent from state to state, such that poor performing providers are held accountable and are not permitted to participate in the Medicare and Medicaid programs.
-
$25 million toward the establishment of Creative Aging Collaboratories: Regional, multi- sectoral public-private partnerships resourced as high-involvement, community service hubs for consumer education and interprofessional, team-based learning in person- directed, relationship-centered community life. These Collaboratories will serve a bridge- building function promoting alignment across the Aging and Disability Services Network, Age-Friendly Health Systems, and the multi-sectoral Age- and Dementia-Friendly Community efforts spreading across the country.
-
$10 million for a national, non-governmental platform to proliferate the culture of well- being and innovation among elders, people living with disabilities (including dementia), and the professionals and organizations (including within government) that exist to support them, including educators and researchers. Similar in form to other collaborative centers funded by the Agency for Community Living (ACL), this community would share information in a multi-level, cross-disciplinary fashion, build networks around specific interests, and provide reality-tested pathways for future research and development. Further study to explore options to financially incentivize nursing homes to transform institutional models by integrating person-directed practices and operations, such as the Kansas PEAK 2.0 pay-for-performance model. (see Using Medicaid Funds to Promote Person-Centered Care in Nursing Homes: A Toolkit for Policymakers) Our nation’s patchwork response to the COVID-19 pandemic has brought into stark relief the fundamental shortcomings in our system of long-term services and supports. The social isolation and loneliness experienced by so many elders and persons living with disabilities including dementia may well have killed more than the COVID-19 disease itself.
As seasoned innovators at the forefront of combatting social isolation and loneliness for decades, the Live Oak Project coalition invites you to join our multigenerational grassroots movement to reimagine, redesign, and transform long-term services and supports in America so that each person can thrive.
Please stand with us and ask government leaders to think bigger and bolder to fund innovative solutions within our communities.
Helen Abel
Margaret Anderson
Casey Acklin
Joe Angelelli
Ashton Applewhite
Barry Barkan
Sonya Barsness
Anne Basting
Jill Battalen
Alice Bonner
Carmen Bowman
Charlene Boyd
KaraLe Causey
Cathie Brady
Chris Bravo
Melora Brooks Jackson
Garth Brokaw
Elisabeth Burgess
Maggie Calkins
Joan Carlson
Kryie S. Carpenter
Jennifer Carson
Hope Carwile
Walter Coffey
Raines Cohen
Al Condeluci
Ann Marie Cook
Mikko Cook
Penny Cook
Mel Coppola
Jennifer Craft Morgan
Evy Cugelman
Joan Devine
Diane Dixon
Amy Elliot
Nancy Emerson-Lombardi
Jonathan Evans
Rose Marie Fagan
Karen Feinstein
Diane Findley
Nancy Fox
Mary Fridley
Terry Fulmer
Rick Gamache
Gary Gibson
Jeni Gipson
Robyn Golden
Julie Gray
Celeste Greene
Demi Haffenreffer
Megan Hannan
Paula Havird
Diane Heliker
Denise Hyde
Beth Irtz
Lynne Iser
Jeff Jerebker
Ruta Kadonoff
Carmelita Karhoff
Betsy Kemeny
Jim Kinsey
Keith Knapp
Pat Kraus
Beverly Kroeger
Dan Kuhn
Jack Kupferman
Emi Kiyota
Bob Lane
Christopher Laxton
Cathy Lieblich
Karen Love
Wendy Lustbader
Richard Machemer
Meredith Martin
Susan Massad
Imelda Maurer
Angie McAllister
Jeff McCabe
Nicolette McDermott-Ketchum
Kim McRae
Vicki Mizel
Anne Montgomery
Rick Moody
Jay Moskowitz
Julie Murawski
Karen Nichols
LaVrene Norton
Michelle Olson
Ric Olson
Anna Ortigara
KJ Page
Karl Pillemer
Jackie Pinkowitz Lori Porter
Allen Power
Liz Prosch
Joanne Rader
Don Redfoot
Peter Reed
Marianne Raimondo
Ray Rusin
Karen Schoeneman
Nancy Schwalm
Penelope Ann Shaw
Steve Shields
Sarah Slocum
John Sorenson
David Sprowl
Irving Stackpole
Karen Stobbe
Brad Stock
Jodi Sturgeon
Vivian Tellis-Nayak
Mary Tellis-Nayak
Bill Thomas
David Troxel
Alice Truluck
Mike Wasserman
Cindy Webb
Paul Winkler
Ann Marie Wyatt
Dan Young
Appendix
Short YouTube video on A Brief History of Person-Centered Care & Culture Change PDF Handout of “A Brief History of Person-Centered Care & Culture Change “
1 Ageism Amplifies Cost and Prevalence of Health Conditions. Levy, BR., Slade, MD, Chang, ES, Kannoth, S, Wang, SY, The Gerontologist, Volume 60, Issue 1, February 2020, Pages 174–181, https://doi.org/10.1093/geront/gny131
2 https://www.wsj.com/articles/nursing-homes-keep-losing-workers-11629898200
3 https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Trends-and- Reports/NationalHealthExpendData/NationalHealthAccountsProjected